Covid-19-vaccination
Contents
Problem definition
Currently, there is a new wave of infection in the COVID-19 pandemic with high number of infections. In Germany, for example, more than 50,000 new infections are currently reported every day. To reduce the infection rate, a wide variety of measures have been implemented. One of these measures are the vaccination and masks. Vaccination can reduce the risk of infection and the likelihood of transmissibility. A simulation is conducted to vividly identify the extent to which vaccination could contain the pandemic.
Method
The purpose of the simulation is to show how COVID-19 vaccination affects the spread of the pandemic. I will use an agent-based model, this method enables to reflect the real scenario at the best. Thereby people can be represented by autonomous agents and it is possible to simulate their daily behavior and thus the spread of the virus in a simplified way.
Model
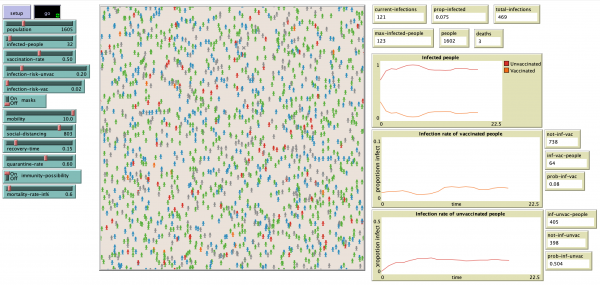
The model shows people in a village. The inhabitants move freely in their village, reflecting their everyday behavior. To simulate the spread of Covid-19, a certain proportion of the population is already unknowingly infected at the beginning of the simulation. As the simulation progresses, they infect their fellow villagers with the virus, allowing it to spread throughout the village. Some of the people are vaccinated. How many among the people are vaccinated defines the particular vaccination rate. Vaccination in this model reduces the risk of infection of a person. To analyze the impact of vaccination on the spread of the pandemic. Several simulations with different vaccination rates are run and their results are compared.
Environment
The model represents an exemplary village in Germany with 1605 inhabitants where the Covid-19 virus is spreaded. For simplification, the village is closed that is new people cannot come in and people of the village cannot go out.
Agents
The people are represented by agents, which have colored blue and have the "people" shape. As mentioned above, a part of the population defined by the vaccination-rate is vaccinated. This property is randomly assigned to the inhabitants. Vaccinated individuals are marked in green. For simplicity, the simulations do not distinguish between different vaccination statuses (1st, 2nd, or 3rd vaccination). In the following, the vaccination rate and the corresponding numbers of the parameters refer to a "complete" vaccination status, i.e. citizens have already received 2 vaccinations.
Movement
People move in a certain radius [mobility] randomly in their environment, this reflects in a very simplified way the behavior of people and their encounters with other people in everyday life, for example, people's way to work, shopping, going to restaurants, etc.
Spread of infection
The initially infected people (marked red or orange in the model) [infected-people] can infect other healthy people with a defined probability if they are in their vicinity. The probability of being infected, i.e. the risk of infection of a person depends on whether he is vaccinated [infection-risk-vac] or unvaccinated [infection-risk-unvac]. The risk of infection is significantly lower for vaccinated individuals, so the likelihood of being infected by a person is lower. Once the person is infected, their color changes. Infected vaccinated persons turn orange and infected unvaccinated persons turn red. For simplification, we do not take into account the incubation period or the time spent with an infected person. In addition, other measures can be set, which are intended to protect against the virus by reducing the risk of infection.
These are wearing a mask and social distancing, these parameters are explained in more detail below. If a person is infected, he or she goes into quarantine with a certain probability. This is simulated in the model in a simplified way, in that the person still moves freely, but can infect other people with a lower probability [quarantine-rate]. After the recovery time [recovery-time], the previously infected person is immune (indicated by the color gray) to the virus [immunity-possibility]. This means that they cannot be infected again. Since infected persons can also die from Covid-19 in the worst case, this is also taken into account in the mortality rate. The mortality rate [mortality-rate] indicates how many of the infected die. Dead persons are marked with an "x".
End of the simulation
The simulation ends when the Covid-19 virus is eradicated from the model village. This means that no more people are infected. This can happen when everyone is immune or so many or so few are infected that the risk of infection approaches 0.
Parameter
Essential model parameter
Infected people at the beginning [infected-people]: An infection rate of 2% is assumed at baseline, corresponding to 35 infected people at baseline. [6]
Vaccination rate [vaccination-rate]: In the following simulation, the spread of the virus is compared with vaccination rates of 0%, 25%, 50%, 75%, 90% and 100%.
Risk of infection of unvaccinated people [infection-risk-unvac]: In reality, different infection risks are found depending on external circumstances. For simplicity, this model assumes that all persons meet indoors and are not at any super-spreader event. Thus, the risk of infection for unvaccinated persons is about 20%. [3]
Risk of infection of vaccinated people [infection-risk-vac]: The probability of contracting Covid-19 is up to 90% lower for vaccinated persons. Since we assume a 20% risk of infection for unvaccinated persons, the risk of infection for vaccinated persons equals 2%. [2]
Mobility [mobility]: reflects the range of motion of the agents in their environment. In the simulations, the largest possible (10) is assumed.
Recovery time [recovery-time]: determines the time it takes an infected person to recover from the disease and become immune. In the simulation, a rate of 0.15 is assumed. The lower the value, the longer the recovery time.
Possibility of immunity [immunity-possibilty]: determines whether people are immunized after infection and can no longer become infected.
Mortality rate [mortality-rate]: defines the percentage of infected people who will die from the virus. For simplicity, we assume that the mortality rate is the same for both vaccinated and unvaccinated people, regardless of external and personal circumstances. The mortality rate is 0.6%. [4]
Further measures for reducing the risk of infection
Masks [masks]: Wearing a mask can reduce the risk of infection to 0.4% in the best case. In the simulations, the best case is assumed, i.e., a fresh mask is worn properly. In addition, this should not bias the analysis around the effectiveness of vaccination in the first simulations. [1]
Social Distancing [social-distancing]: This parameter describes the number of people who engage in social distancing at the beginning of the simulation. This is reflected in a simplified model by the fact that the persons do not move. Since there is currently no lockdown, we do not assume this for the time being in the simulations and set social distancing to 0. In addition, this should not distort the analysis of the effectiveness of the vaccination.
Quarantine [quarantine-rate]: determines the probability that an infected person cannot infect another person, because he is in quarantine. Even in reality, not every person is in quarantine because, for example, they do not show any symptoms and thus no suspicion of Covid-19 arises that could lead to quarantine measures. It is estimated that approximately 40% of those infected do not quarantine. Thus, the quarantine rate corresponds to 60% in the simulations. Duration of quarantine corresponds to recovery time. [5]
Output
Plots
Results
Vaccination rate: 0%
Vaccination rate: 25%
Vaccination rate: 50%
Vaccination rate: 75%
Vaccination rate: 90%
Vaccination rate: 100%
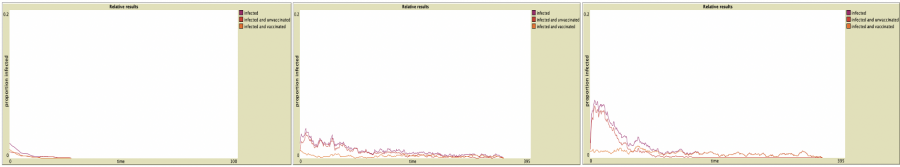
Simulation with further measures
For the simulations with measures, a vaccination rate of 50% was assumed. Subsequently, the individual measures: Masks, Quarantine and Social Distancing were applied. The results show that the measures can again reduce the infection rates. Especially the mask is an effective measure (plot 1). This prevents a steep rise in infections and thus significantly reduces infections. This also shortened the duration of the pandemic. However, it should be taken into account here that the simulation assumed the best case scenario. Another measure that works is quarantine. An increase in the quarantine rate leads to a flatter course of the infection curve (plot 2). Social distancing, on the other hand, reduces infection rates only slightly in this mode and is thus the weakest of all measures (plot 3). The measures are equally successful for both vaccinated and unvaccinated. The vaccination status does not influence the effect of the measures.
Conclusion
As expected, the results show that vaccination against COVID-19 has a positive impact on the spread of the virus. Similarly, the different vaccination rates affect the pandemic in different ways. Although vaccination prolongs the duration of the pandemic, fewer people become infected with the virus during it, even at low vaccination rates. Among the uninfected at the end of the pandemic, there are only vaccinated people. Conversely, this means that unvaccinated individuals have a 100% probability of becoming infected with COVID-19 during the pandemic. The infection rate among vaccinated individuals and unvaccinated individuals follows a similar trajectory regardless of vaccination coverage. The trajectory of total infection rates approaches either the infection rate among vaccinated individuals or unvaccinated individuals, depending on the vaccination rate. If the vaccination rate is low, the COVID-19 virus spreads rapidly at the beginning of the pandemic, meaning that infection numbers increase rapidly and decrease as the pandemic progresses. The higher the vaccination rate, the slower the virus spreads, resulting in a flat curve of infection numbers. As a result, the number of infections is significantly lower and relatively constant at the beginning. Although, despite the high vaccination rate, over 90% still become infected during the course of the pandemic, vaccination avoids a rapid spread of the virus and thus extremely high infection numbers. This can be helpful, for example, with regard to the capacity of hospitals and intensive care units, as they do not have to care for a large number of people at once and thus reach their limits. In addition, other measures, such as masks or quarantine, help to further contain the virus. For example, the quarantine rate can be increased by regular COVID-19 testing. In addition, the risk of infection depends on the environment and COVID-19 variants. By adjusting the infection risks, the simulation can be run again with different infection probabilities and compared.
Sources
Bagheri, G., Thiede, B., Hejazi, B., Schlenczek, O., & Bodenschatz, E. (2021). An upper bound on one-to-one exposure to infectious human respiratory particles. Proceedings of the National Academy of Sciences, 118(49), e2110117118. [1]
Harder, T., Külper-Schiek, W., Reda, S., Treskova-Schwarzbach, M., Koch, J., Vygen-Bonnet, S., & Wichmann, O. (2021). Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection with the Delta (B.1.617.2) variant: Second interim results of a living systematic review and meta-analysis, 1 January to 25 August 2021. Eurosurveillance, 26(41). [2]
Lelieveld, J., Helleis, F., Borrmann, S., Cheng, Y., Drewnick, F., Haug, G., Klimach, T., Sciare, J., Su, H., & Pöschl, U. (2020). Model Calculations of Aerosol Transmission and Infection Risk of COVID-19 in Indoor Environments. International Journal of Environmental Research and Public Health, 17(21), 8114. [3]
Meyerowitz-Katz, G., & Merone, L. (2020). A systematic review and meta-analysis of published research data on COVID-19 infection fatality rates. International Journal of Infectious Diseases, 101, 138–148. [4]
Oran, D. P., & Topol, E. J. (2020). Prevalence of Asymptomatic SARS-CoV-2 Infection: A Narrative Review. Annals of Internal Medicine, 173(5), 362–367. [5]
Sun, C., & Zhai, Z. (2020). The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustainable Cities and Society, 62, 102390. [6]